Introduction
Acute chest syndrome (ACS) is a clinical presentation of fever, chest pain, pulmonary symptoms, and new infiltrates on lung imaging. It affects nearly 50% of patients with sickle cell disease during their lifetime and often leads to hospitalization. The mortality rate is variable ranging from 3 to 9 %. and depends on several factors. We aimed to identify the clinical and epidemiological characteristics of patients admitted with ACS on a national scale and factors affecting clinical outcomes in inpatient setting.
Methods:
We utilized the National Inpatient Sample (NIS) database 2019 for the purpose of this study. Using this database, we identified patients with a principle diagnosis of ACS using International Classification of Diseases (ICD-10) codes. Data on demographic characteristics such as age, sex, race, insurance type were collected. Additionally, we selected clinically significant medical comorbidities such as asthma, chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD), chronic kidney disease (CKD), heart failure, hypertension, diabetes mellitus (DM), sepsis, obesity, and others. The primary endpoint of this study was to identify factors influencing all-cause mortality, while the secondary endpoint was to identify factors influencing mechanical intubation, in-patient blood transfusion, and length of stay. We used multivariate logistic regression analysis to adjust for confounders. A p value of ≤0.05 considered statistically significant.
Results:
Baseline Characteristics
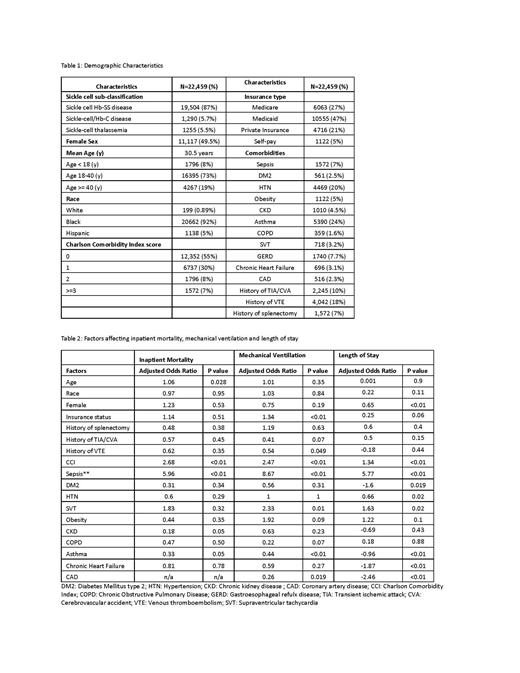
Our analysis consisted of 22,459 patients who were admitted with principal diagnosis of ACS. 49.5% were female and 50.5% were male. Mean age was 30.5 years. African American race was predominant (92%) with sickle cell Hb-SS disease (87%). Major insurance payer was Medicaid (47%) followed by Medicare (27%) and then private insurance (21%). Asthma was the most common comorbidities (24%) and majority of patient had Charlson Comorbidity Index (CCI) score of zero (55%). The details of clinical and epidemiological characteristics are shown in Table 1.
Clinical outcomes and factors influencing mortality
Only 0.89% patient died of ACS. Average length of stay was 6.86 days. 34% of the patient required packed red blood cell (pRBC) transfusion. 3.2% needed mechanical ventilation. In multivariate analysis, factors associated with mortality included age of patient, CCI and sepsis. Younger patient had higher odds of mortality however this was not statistically significant. There was no difference in mortality with sex, race and insurance status of the patients.
Factors affecting inpatient transfusion, mechanical ventilation and length of stay
Female, higher CCI score and sepsis on admission were associated with higher needs of inpatient pRBC transfusion. Within race, White (OR 3.16, CI 1.44-6.93, P <0.01) and Hispanics (OR 2.68, CI 1.59-4.51, P<0.01) had higher odds of receiving transfusion compared to African Americans (OR 1.84, CI: 1.17-2.89, P <0.01). Similarly patient with sepsis, supraventricular tachycardia had more odds of needing mechanical ventilation. Patient's insurance status was also related to increased odds of intubation. Comorbidities such as asthma and CAD were not associated with need of mechanical ventilation and in fact our study shows they had less odd of needing mechanical ventilation. Length of stay was influenced by several of epidemiological and clinical comorbidities. Females had less odds of longer length of stay compared to male (OR: 0.65, P <0.01). Comorbidities such as asthma, heart failure, CAD, DM2 and hypertension did not increase the length of stay while patients with sepsis and high CCI score had higher odds of hospitalization for extended period of time. The details are in Table 2.
Conclusion
We found mortality was 0.89% in patients admitted with ACS compared to 3 to 9% previously reported. Sepsis and CCI were one of the predictors for odds of having higher mortality, need of blood transfusion, mechanical ventilation and increased length of stay in patient with ACS. Female, White and Hispanic had higher odds of needing transfusion then African Americans. Comorbidities such as asthma, heart failure, CAD, DM 2 and hypertension did not increase the odds of prolonged hospital stay.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal